Are you tired of living with constant pain that hinders your quality of life? Look no further than Medical Pain and Spine Care, where our dedicated team of experienced healthcare professionals is committed to helping you find relief. We understand the physical, emotional, and psychological toll that chronic pain can take on you, and we’re here to provide compassionate care and effective solutions tailored to your unique needs.

STEP TOWARDS A LIFE
WITH LESS PAIN

STEP TOWARDS A LIFE
WITH LESS PAIN

STEP TOWARDS A LIFE
WITH LESS PAIN

Text or call Us Today
Don’t let pain hold you back any longer. Call our pain clinic today to schedule a consultation and embark on your journey towards a pain-free future. Fax us at 317-773-7910
Message Us Today
Our secure messenger is designed with advanced encryption protocols and robust security features to safeguard your sensitive information and ensure that your conversations remain private.
Our Hours
-
Monday - Thursday8:00 - 5:00 PM
-
Friday8:00 - 12:00 PM
-
Closed for Lunch12:00 - 1:00 PM
-
Saturday & SundayClosed
-
EmergencyContact 911
Our Treatment Options
At Medical Pain & Spine Care of Indiana, treatment options may include spine procedures, muscle and joint injections, pain management device implants, medication management, wellness options and even medical weight loss which can improve joint and lower back pain.
spinal cord stimulation intrathecal drug pump therapy
Pain Pump
(Intrathecal drug pump)
Peripheral Nerve Stimulation
Spinal Cord Stimulation
Ketamine Infusions
Ketamine has been used safely as an anesthetic for over 50 years. Ketamine infusions are used to treat mood and pain disorders.
Platelet Rich Plasma (PRP) Therapy
Packed with growth and healing factors, platelets initiate repair and attract the critical assistance of stem cells.
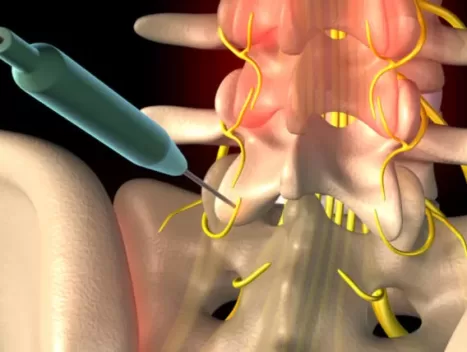
Cervical, Thoracic, and Lumbar Spine Procedures
- Epidural Steroid Injections
- Spinal Nerve Blocks
- Spinal (facet) Joint Blocks
- Sacroiliac Joint Injections
- Radiofrequency Ablation
Intracept Procedure
The Intracept procedure is a revolutionary and minimally invasive treatment option for patients suffering from chronic low back pain.
headache and migraine Botox
If you suffer from chronic migraines that significantly impact your daily life, Botox treatment may offer much-needed relief and a path towards a better quality of life.
Cosmetic Botox
The first and only treatment FDA approved to temporarily make moderate to severe frown lines, crow’s feet, and forehead lines look better in adults.
Wellness Options
- B 12 Injection
- Lipostat Plus
- Get-Up-And-Go Infusion
- Hangover/ Headache Infusion
- Quench Infusion
- Immunity Infusion
- Myers Cocktail
What is Ketamine?
What is Ketamine?
Ketamine is a powerful medication that has gained significant attention in recent years for its potential in treating various medical conditions, particularly in the field of pain management and mental health. Originally developed as an anesthetic, ketamine has shown remarkable therapeutic effects beyond its traditional use.
How Can Ketamine Help you?
Click here to see how Ketamine can help you .
High success rate


Each Patient Has a Unique Story
At Medical Pain & Spine Care, we strive to show patients how much we care about them. Our providers take time to listen to each patient’s story and then provide an individualized treatment plan to produce maximum pain relief.
- Medical Pain & Spine Care prioritizes patient care and aims to demonstrate genuine concern for each individual.
- The providers at Medical Pain & Spine Care dedicate time to attentively listen to every patient's unique story, understanding their concerns and needs.
- By comprehending each patient's story, Medical Pain & Spine Care develops personalized treatment plans tailored to their specific condition and requirements.
- The primary goal of the individualized treatment plans is to achieve the highest level of pain relief for each patient, ensuring their comfort and well-being.
- Medical Pain & Spine Care believes in the power of customized care, recognizing that a one-size-fits-all approach may not be effective in addressing diverse pain conditions.
Meet Our Providers
J Peter Klim, DO
board certified pain management physicianHaylee Goad, FNP
NURSE PRACTITIONEREmily Hackett, FNP-C
NURSE PRACTITIONERNews and Research
- Medical Pain and Spine Care
- 0 Comments
Discover the Klim Comfort Method™ — A Gentle, Proven Approach to Interventional Pain Management in Noblesville
If fear of painful procedures or injections has kept you from seeking care, you’re not alone. At our pain management clinic in Noblesville, Indiana, we hear it all the time: “I’ve just learned to live with the pain.” “I’m afraid it’ll hurt more than it helps.” “I don’t like needles.” That’s exactly why Dr. Peter […]
- Medical Pain and Spine Care
- 0 Comments
Intravenous Lidocaine: A Promising Option for Fibromyalgia Pain Relief
Facebook Recent research highlights intravenous lidocaine (IVL) as a promising option for reducing pain in fibromyalgia (FM) patients, especially when traditional treatments like antidepressants lose effectiveness or cause side effects. A review of 10 studies with 461 patients found short-term pain relief with IV lidocaine, with VAS pain scores dropping significantly after treatment. While side […]
- Medical Pain and Spine Care
- 0 Comments
Mindfulness Meditation and Placebo Modulate Distinct Neural Signatures to Reduce Pain
Facebook Mindfulness meditation, which has been used for pain management in various cultures for centuries, has long been thought to work by activating the placebo response. Now new research demonstrates that its effectiveness actually comes from engaging distinct brain mechanisms to reduce pain compared with those of the placebo response. The research, published in Biological Psychiatry (2024: S0006-3223[24]01556-7), […]
- Medical Pain and Spine Care
- 0 Comments
Emotional Awareness, Expression Therapy Shown to Curb Pain Severity
Facebook A randomized clinical trial’s results suggest that emotional awareness and expression therapy (EAET) “may be a preferred intervention for medically and psychiatrically complex patients with pain.” The study was conducted between 2019 and 2023 at the Veterans Affairs Greater Los Angeles Healthcare System (VAGLAHS) and represents the first full-scale evaluation of EAET (JAMA Netw Open 2024;7[6]:e2415842). It […]
- Medical Pain and Spine Care
- 0 Comments
Psychosocial Distress May Be Best Indicator of High-Impact Chronic Pain With KOA
Facebook Data published in the Journal of Pain indicate that high-impact chronic pain (HICP) is more common among people with knee osteoarthritis (KOA) when pain is assessed by its effect on physical function rather than pain interference scores. However, psychosocial distress was found to be a consistent feature of HICP, regardless of the pain assessment method. […]
- Medical Pain and Spine Care
- 0 Comments
Trim the Fat, Reduce the Pain?
Facebook A first-of-its-kind study has found a link between carrying extra fat in the gut and widespread chronic pain, with reductions in body fat correlating with lessening pain.Reducing excess body fat in multiple areas was further linked to more reductions in pain—with the association between excess abdominal fat and chronic pain strongest in women, according […]
- Medical Pain and Spine Care
- 0 Comments
Multiple Benefits From Remote SCS Management in Chronic Pain Patients
LAS VEGAS—new research has uncovered several benefits associated with remote management of spinal cord stimulators, including a reduction in patient burdens and improvements in care. Interim results from the prospective, multicenter BENEFIT-03 study showed remote device management to be a highly useful tool, one that was well received by both patients and their clinicians. Read […]
- Medical Pain and Spine Care
- 0 Comments
Peptides: A promising alternative to opioids for chronic pain relief
A novel peptide for pain relief The researchers developed a novel peptide molecule that could prevent endocytosis to reduce the hyperactivity of these pain neurons and thereby minimise pain perception. “This novel peptide molecule is a lipidated endocytic dileucine sequence found in the human CD4 protein known to bind to the AP2 complex at the […]
- Medical Pain and Spine Care
- 0 Comments
Top Celebrities Who’ve Had PRP Treatments
Facebook Our country wasn’t the first to adopt PRP. Kobe Bryant had to run to Germany to get his first PRP treatment. And his success and his raving about his success contributed heavily to PRP’s skyrocketing popularity now. In fact, he’s the one who told Alex Rodriguez to get his PRP. Bryant is indeed the […]
- Medical Pain and Spine Care
- 0 Comments
Trial of Cooled Radiofrequency Ablation
Facebook Lumbar medial branch radiofrequency ablation (LRFA) and intraarticular facet steroid injections (FJI) are commonly performed for recalcitrant facet joint-mediated pain. However, no study has compared clinical outcomes of the two treatments in patients selected using dual medial branch blocks (MBBs) with an 80% relief threshold. Read the results at Oxford Academic. More to explorer